A new, rapidly spreading variant of SARS-CoV-2, the virus that causes COVID, means a rise in new infections could be around the corner. And while it likely won’t skirt immunity completely, the variant could dodge some of our defenses thanks to a mutational boost.
XBB.1.5—unofficially nicknamed “Kraken” by some scientists online—is an Omicron subvariant that has caught the attention of virologists in recent weeks because of its significant advantage in how fast it spreads. Research by computational virologist Trevor Bedford and his team at the Fred Hutchinson Cancer Center in Seattle suggests XBB.1.5 currently has a reproduction number of around 1.6, meaning that every person infected by this subvariant will, on average, go on to infect about 1.6 other people.
“According to the Centers for Disease Control and Prevention’s Nowcast estimates of variant proportions, XBB.1.5. is likely already among the most prevalent subvariants in the U.S.,” says Marlin Figgins, a University of Washington Ph.D. student working in Bedford’s lab. “It’s likely there will be an increase in cases in the short term, though this will depend on the extent of XBB.1.5’s advantage and the various factors affecting SARS-CoV-2 transmission in general.”
Crucially, despite being a few dozen mutations away from the subvariant BA.5, which dominated last summer, XBB.1.5 is still a form of Omicron and not some completely new SARS-CoV-2 variant. It is also very similar to its parent lineage, XBB—itself a combination of two lineages descended from the subvariant BA.2 that dominated last spring.
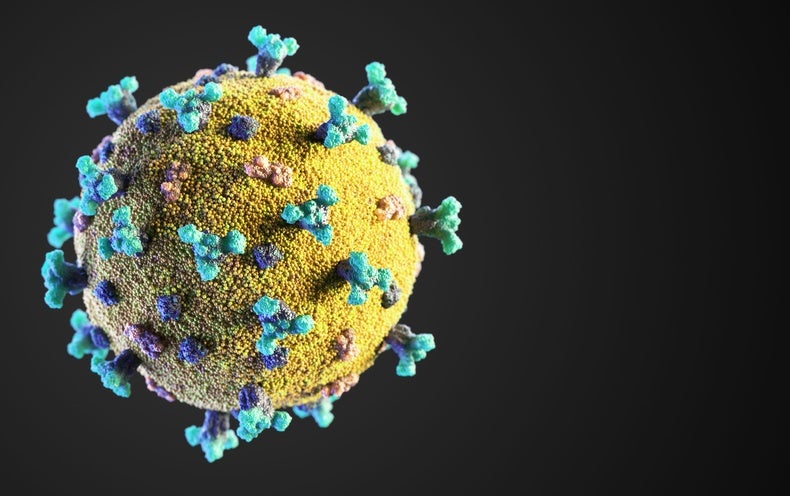
The parental XBB, which made headlines after causing a wave of infections in Singapore last year, is notable for its ability to evade the human immune system using a mutation at a site on its spike protein known as 486. Mutations at this site are known to have helped the virus escape detection by the immune system even in its earliest variants in the pandemic. Lawrence Young, a professor of molecular oncology at the University of Warwick Medical School in England, describes the mutation as an evolutionary trade-off: “It provides for more immune evasiveness, but it [is a] trade-off in terms of infectivity in that the change makes the virus slightly less efficient for infection,” he says.
By contrast, XBB.1.5’s defining feature and its main difference from XBB is a spike protein mutation known as F486P. This mutation gives XBB.1.5 a significant advantage, boosting infectivity while retaining XBB’s ability to sneak past human defenses. In other words, it’s less of a trade-off and more of a turbocharge.
The mechanism behind XBB.1.5’s increased transmissibility isn’t known for sure. But the subvariant’s F486P mutation allows the virus to more effectively latch onto ACE2 receptors in the body—“the doorway through which the virus gets into cells in our noses, throats and lungs,” Young says.
“I think few studies show a direct correlation between ACE2 binding and being better able to transmit” the virus, says Stanley Perlman, a professor of microbiology and immunology at the University of Iowa. “I’m sure it’s a factor, but it’s just one of many factors.”
The result is that XBB.1.5 is highly transmissible while retaining Omicron’s ability to evade the immune system. Several experts have stressed that XBB.1.5’s immune evasion properties should not be overstated, however. While the subvariant may, to some extent, dodge antibodies conferred by vaccines or prior exposure, it will not skirt the immune system completely, says Alessandro Sette, a professor at the La Jolla Institute for Immunology. Sette says XBB.1.5 would have a hard time escaping the cellular immunity conferred by killer T cells, which work by destroying virus-infected cells even if antibodies fail to stop those cells from being infected in the first place. This T cell response helps prevent severe disease. There is currently no evidence to suggest that XBB.1.5 causes more or less severe disease or different symptoms, compared with previous Omicron subvariants.
“There has been significant confusion in the narrative of protection,” Sette says. “It’s relatively easy for a virus to mutate to escape antibodies because they are limited to a certain area of the virus’s spike protein. But what about cellular immunity? The mechanism by which T cells recognize the virus is completely different.” He adds that while certain SARS-CoV-2 variants can escape antibodies to varying degrees, T cells retain about 85 percent of their ability to fight against the virus at the population level.
This reinforces a point many experts have made throughout the pandemic: even though immunity from vaccines or prior exposure may not prevent people from being infected multiple times, it will still help to prevent serious illness.
Jake Scott, a clinical assistant professor of infectious diseases at Stanford University, is not concerned about XBB.1.5 yet. “I believe it is clear that all the subvariants of Omicron are intrinsically less likely to lead to severe disease because they’re less likely to lead to lower respiratory tract disease,” he says. “Yes, the Omicron subvariants are quite transmissible, and yes, XBB.1.5 is the most transmissible of the Omicron subvariants, so it is possible that it will lead to a rise in cases. But I really have no concern that it is going to lead to a rise in hospitalizations and deaths that are solely due to COVID.”
Scott acknowledges that this is mostly conjecture. “But even though I’m reluctant to make any predictions, I think it’s okay to have confidence in vaccines,” he says.
Sette echoes that point: “Certainly there have been tremendous waves of infection with each different variant, but to a large degree, the vaccines have held their protection against severe disease,” he says. “Now we have bivalent boosters that are even better—that’s very important.”
What’s more, antiviral COVID medications such as Paxlovid and remdesivir “should still be effective against XBB.1.5,” Young says. “Both of these will prevent virus replication, and their crucial function is not altered in XBB.1.5.”