Several years ago, I was at a pre-season football practice at a high school where I was working with the team on a concussion research project. The players were lined up in two rows facing each other and with little more instruction from the coach than, “on the whistle, hit the man across from you,” grave concern rushed through my mind.
Professional sports get the lion’s share of attention, but concussions are a significant medical issue at all levels of play. While roughly 1,700 athletes play professional football each year, over three million children and adolescents in the United States play the same game. This squarely places concussions as a significant public health concern in homes from coast to coast.
For decades, athletes, parents, coaches and medical professionals considered concussion a temporary injury with no long-term consequences. Athletes commonly played through it as a sign of toughness. Our thinking on concussion shifted around 2005, when the brain tissue pathology report of Mike Webster, a retired National Football League player, was published. The report was the first to identify chronic traumatic encephalopathy (CTE) in a football player and suggested the disease was linked to concussions the player had suffered on the field. Since then, public attention has focused on this link between brain injury and blows to the head, and much of that conversation has centered around football.
Participation in any sport carries injury risk, and concussion will always be part of that calculus. This was never more evident than early in the 2022 season, when Miami Dolphins quarterback Tua Tagovailoa was concussed while playing against the Cincinnati Bengals, his contorted hands on full display in front of a national audience. Concussion prevention and care is better now than it has ever been, but short of ending all sports, we need to do more to prevent them. This means improvements in equipment, better training for coaches and players, and better medical care.
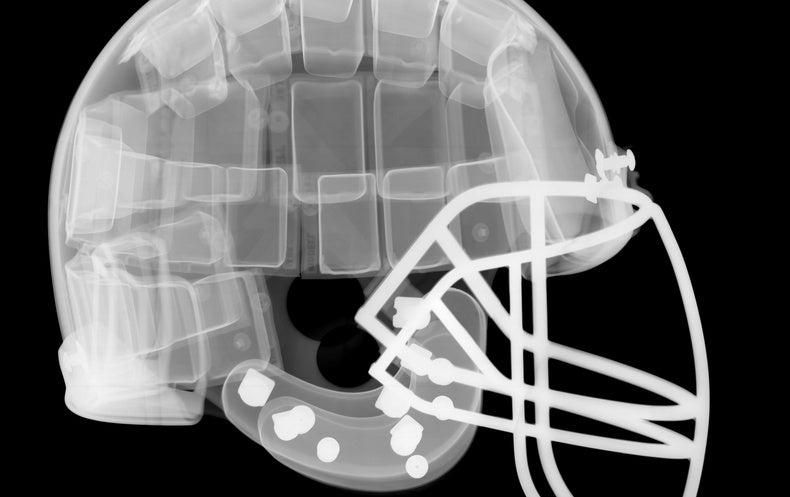
In the early 1900s football was played without helmets, but severe injuries, like skull fractures, lead to the sporadic use of leather helmets in the 1920s. The plastic shell helmet was invented in 1939 and became mandatory a few years later. The first face mask entered the game in the 1950s, and foam padding wasn’t added until the 1960s. Over the years, engineers updated the basic design with more robust face masks and newer internal padding such as air bladders and gel padding. Until recently, these changes were all made with an eye toward reducing the most severe brain injuries such as brain bleeds and skull fractures, and they have been largely successful. But as our understanding of concussion evolved to understand its significance as an injury, so too did the scrutiny of player equipment.
The fundamental problem is that regardless of how much impact force is mitigated by protective equipment, we cannot stabilize the brain inside the skull following an impact – likely making a concussion-proof helmet an impossible engineering challenge. That hasn’t stopped helmet improvements, however. With a new eye toward concussion prevention, researchers at Virginia Tech introduced a helmet rating system specific to concussion risk in 2011. The five-star system (one being the worst, five the best) rates the ability of the helmet to reduce concussion risk. This gives consumers tangible evidence to make an informed purchase. In its first year, only a single helmet was awarded a five-star rating, but now, the most recent rankings list more than 25 five-star helmets. Modern helmets use advanced shell materials that flex upon impact, have moveable panels to absorb forces, and multi-layered padding that responds to different impact velocities. Companies will continue to improve helmets as new materials become available, guided by the newest science.
But engineering limitations should not stop us from closely examining other factors that can reduce concussion risk. For example, in one study of head impacts and concussion across five college football seasons, nearly 50 percent of concussions occurred during the four-week pre-season; the rest occurred over the next 12 weeks of in-season play. Such data led the NCAA to reduce the number of allowable full contact pre-season practice sessions. Others have shown that reducing the number of high school football practices in which contact is allowed reduces head impacts by as much as 46 percent. Moving the kickoff line forward to the 40-yard line reduced the number of times the ball is run back by the receiving player. This is one of the riskiest plays of the game in terms of concussion.
As players get older and start playing contact football, the coaching staff must teach appropriate tackling technique—not leading with the head and wrapping their opponent up with their arms. Learning how to do this properly has the added benefit of more playing time (i.e., you can’t play if you’re injured). In addition, having medical providers with training in concussion management at practices and competitions can help identify and rapidly remove injured players, a known factor in reducing injury severity and the time out of sport.
While injury prevention is the best approach, concussions will always be a part of sport participation. This is broader than just football. This injury occurs in all sports and affects athletes regardless of sex. Women, who make up about 45 percent of college athletes, tend to report more concussions in sex-comparable sports, but represent only 20 percent of the medical literature. Some researchers have speculated women are more likely in general to report a medical concern to a health provider, but they also have smaller neck musculature relative to their head mass limiting their ability to stabilize their head when hit. Some data indicate an increased risk of concussion at different points in the menstrual cycle. This all suggests that concussion is not unique to football and unless we intend to ban all sports, it is urgent that we continue working to better understand concussions and how to prevent them.
In the interim, several medical and organizations have created concussion guidelines that did not exist in the early 2000s, and every four years a group of international experts meets to review the relevant medical literature and make recommendations on the best approach to concussion care. The latest guidelines are due later this year. Like all medical advances, change will be incremental and often hard to perceive, but concussion prevention and care is better now than it has ever been. Regardless, many athletes will do just about anything to stay on the field and “play through the pain.” It is imperative to create a culture that supports athletes and encourages them to come forward when injuries happen, empowers them to be their own health advocates, and allows them to protect their overall brain health while playing competitively and safely.
Change is happening in how we view sports-related concussions. In my 20 years of doing concussion research, I can attest that we now take concussion seriously as an injury, better understand impact biomechanics and other risk factors, are making strides to prevent it, and are improving the management and recovery process. Sports are an integral part of American culture, and they give millions of children much-needed exercise. As those children become adults and make sport their hobby or even vocation, ensuring they play safely at all levels is essential.
This is an opinion and analysis article, and the views expressed by the author or authors are not necessarily those of Scientific American.