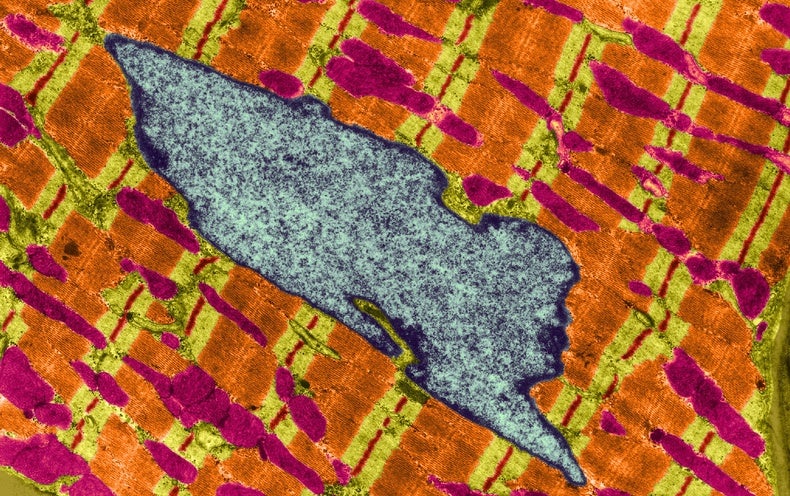
Healthy mitochondria, those tiny cellular structures high school biology teachers often tout as “the powerhouses of the cell,” are a necessity for producing energy in the body—but new research supports the idea that they are more than just adenosine triphosphate (ATP)–pumping machines. For about a decade, scientists have experimented with transplanting these microscopic organelles to treat damaged hearts and other tissues, and they have seen a handful of successful outcomes in human trials. But the role mitochondria play in the healing process is still a mystery.
“There’s an entire field of basic science that just is begging, like, ‘Please, please, please come and explore here,’” says Lance Becker, a resuscitation medicine researcher at the Feinstein Institutes for Medical Research in Manhasset, N.Y.
In a recent study in rats published on March 16 in BMC Medicine, Becker and his colleagues found that a single injection of mitochondria into a blood vessel after resuscitation from cardiac arrest could boost both survival rates and neurological outcomes. Within just 15 minutes of the injection, the researchers saw improvements in the rats’ levels of lactate and glucose—biomarkers associated with tissue healing and neurological recovery—and found evidence that some of those mitochondria reached the brain. The study authors also found the transplanted mitochondria in several other organs, such as the kidneys, suggesting that the organelles had moved from the injection site and were taken up by various tissues throughout the body.
“It’s great that they were able to get it into neural cells,” says Boston Children’s Hospital cardiac surgery researcher James McCully, who was not involved in the study. He adds that in his past work, he hadn’t seen mitochondria move so far from the injection site. “It’s a big step forward, and it’d be nice if this systemic application can be converted to a larger animal model,” McCully says.
In humans, cardiac arrest is fatal in 90 percent of cases, and the 10 percent of people that do survive often have neurological damage. Evidence that the injected mitochondria could travel to the animals’ brain “opens up a whole new area of treatment for patients coming in with neurological defects and neurotrauma [head and spin injuries],” McCully says.
During mitochondria transplantation, organelles from an uninjured muscle are harvested and injected near damaged tissue or into a blood vessel. Blood carries the functional mitochondria to tissues, where they are absorbed, and then the healing process ramps up. While an increase in accessible energy—in the form of ATP—probably helps the body heal, Becker suspects the organelles could be contributing in another way as well. The new mitochondria might also be sending out signals to trigger cell repair, alter metabolism or coordinate activity of existing host mitochondria, he says.
Some of the earliest research on mitochondria transplantation began in animal models at Boston Children’s Hospital, where researchers noticed that heart tissues that could not heal properly often contained cells with damaged mitochondria. Because it wasn’t feasible to directly fix the existing damaged organelles, McCully and his colleagues decided to try introducing healthy mitochondria to take over energy production and launch repair. After experiments in pigs, in 2015 McCully and cardiac surgeon Sitaram Emani of Boston Children’s performed the first human trials on infants who had suffered rare complications after heart surgery that couldn’t be addressed with existing treatments. Over the course of three years and 12 patients, the technique restored healthy cardiac function in the hearts of eight babies.
One of the therapy’s big mysteries is whether the functioning mitochondria themselves are directly responsible for the recovery outcomes or if other proteins and molecules, such as the lipids and carbohydrates that make up the mitochondria, have an impact. To unpack what happens after the mitochondria injection, Becker and his team induced cardiac arrest in 33 rats for 10 minutes and then resuscitated them. During cardiac arrest, the animals experienced tissue damage from the lack of oxygen and nutrients throughout their body, including their brain.
Then Becker and his team injected one of three solutions into veins in the rats’ hind legs: freshly isolated mitochondria from donor rats, frozen and thawed mitochondria from donor rats or a buffer solution without mitochondria. The frozen mitochondria solution contained the same proteins, DNA and carbohydrates that make up the organelles, but the mitochondria themselves were no longer fully functional because of freeze damage, Becker explains. If these injections also helped the rats heal, it would suggest that the building blocks of mitochondria, not the working mitochondria themselves, were driving the recovery process.
The team found that the rats’ survival rates significantly increased, compared with the other two groups, when the animals received infusions of fresh mitochondria. Three days after the cardiac arrests, 10 of the 11 rats that were given fresh mitochondria were still alive while only six of 11 rats in each of the groups that had received one of the other two mixtures survived that long. Moreover rats that received the fresh mitochondria had better neurological function and cerebral blood flow than the animals in the other groups.
Becker’s team also marked some of the transplanted mitochondria with fluorescent dye and found them in the rats’ brain, kidneys and spleen 24 hours after the procedure. But the team doesn’t know their specific path from the bloodstream to these locations.
Christoph Maack, who studies cellular defects in heart failure at University Hospital Würzburg in Germany, is skeptical that such transplants introduce working mitochondria into cells, despite the new research. “There are many studies that show benefits of the method, but we are not convinced that these benefits can be achieved by mitochondria entering cells and functioning there,” he says. In 2020 Maack conducted a study that suggested that before mitochondria entered the heart muscle, they would swell and burst in the bloodstream as a result of a calcium overload in the chemical environment outside of cells.
As researchers continue to probe the mechanism behind mitochondria transplants’ effectiveness, many are also forging ahead to discover more areas where the technique can be helpful. Since the initial mitochondria transplants in infants, other labs have started trials in humans, including in stroke patients. And according to Emani, “the next real opportunity for us will be in the [organ] transplant world.” He and his colleagues aim to get approval from the U.S. Food and Drug Administration to test how mitochondria might revive harvested organs that would otherwise be deemed unfit to transplant into another human.
For mitochondrial transplants to treat common conditions such as cardiac arrest and stroke, which require the fastest treatment possible, it may not be practical to wait for a specially trained scientist to extract mitochondria from a person’s muscle and prepare it for infusion. Instead Becker imagines a hospital might maintain a mitochondria bank, similar to a blood bank, containing readily available organelles from volunteer donors. It’s not clear yet what criteria would make a person a good mitochondria donor, Becker says, but the organelles could be generated from lab-grown cells cultured in dishes.
“Ideally what we would have is a cellular source of mitochondria that grows in every hospital,” Becker says.