Lyme disease, also known as Lyme borreliosis, is an infection spread to humans through the bite of blacklegged ticks carrying a type of bacteria called Borrelia burgdorferi, or very rarely, B. mayonii.
Common symptoms include a erythema migrans rash (often shaped like a distinctive “bullseye”), fever, fatigue and headaches. Without treatment, the infection can spread to the heart, joints and the nervous system, according to the Centers for Disease Control and Prevention (CDC).
In the United States, approximately 476,000 people may get this condition each year, according to the CDC.
Although Lyme disease can be caught all year round in the U.S., ticks are most active between April and October. In some locations, up to half of the local tick population can carry B. burgdorferi. Most U.S. states have reported cases of Lyme disease, but states in the Northeast, upper Midwest and Northwest tend to be most affected, according to Johns Hopkins Medicine.
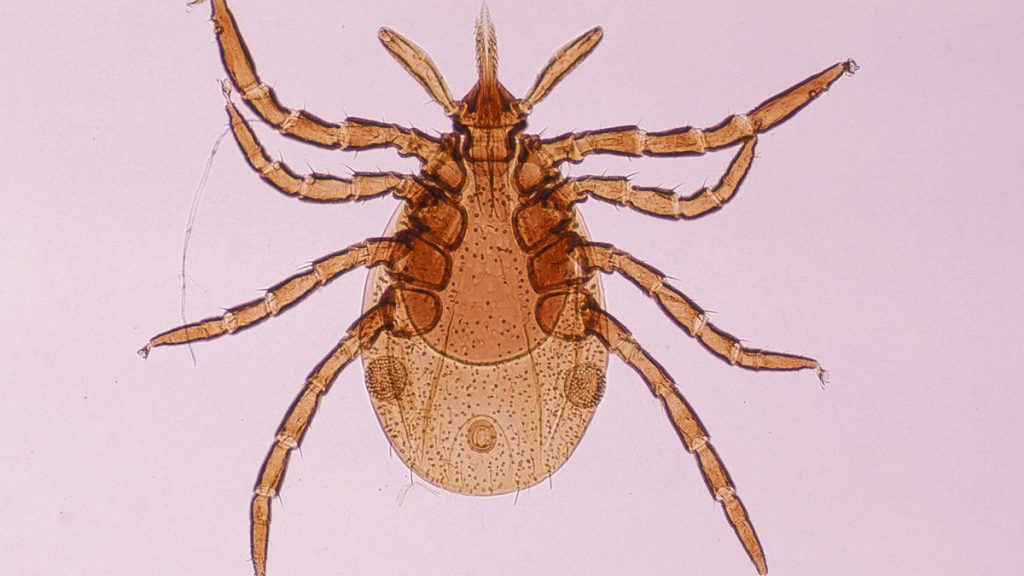
Lyme disease is primarily spread by the blacklegged tick, or deer tick (lxodes scapularis), in the northeastern, mid-Atlantic, and north-central United States, and by the western blacklegged tick (l. pacificus) in the Pacific Coast states, the CDC said.
Related: Your skin should be toxic to ticks. Here’s why it’s not.
Antibiotics like doxycycline and amoxicillin can be effective treatments for early Lyme disease. (Image credit: Science History Images / Alamy)
What are the symptoms of Lyme disease?
The most common symptom of Lyme disease is the so-called bullseye rash, or erythema migrans rash. Often the first sign of Lyme disease, the oval-shape rash spreads gradually from the site of the tick bite in a widening circle. It forms within seven days after an individual is bitten, on average, and can persist for several weeks.
Around 70% to 80% of Lyme disease patients have such a rash. However, some people who have the rash may not notice it, said Dr. Gary Wormser, the chief of the Division of Infectious Diseases and head of the Lyme Disease Center at New York Medical College in Valhalla, New York.
“It is not particularly itchy or painful in most patients. If you do not look at your body that frequently, you may miss it,” Wormser told Live Science.
The rash usually clears up on its own in about four weeks, but the bacteria causing the infection linger even after the bullseye disappears, Wormser said. Lyme disease patients who do not get treated right away may have other symptoms as the bacteria spread through the bloodstream.
Days to weeks after the tick bite, individuals may experience fever, fatigue, aches and pains, Wormser said. According to Johns Hopkins, headache, neck stiffness, swollen glands and poor appetite can also occur at this stage of infection. These symptoms often disappear on their own, leading individuals to think they are no longer sick, Wormser said.
Related: 9 out of 10 ticks in this Pennsylvania park carried a potentially fatal neurological virus
Eventually, new, more severe symptoms can emerge, but they may do so weeks, months or years after the initial bite. These symptoms stem from inflammation in the heart, eye and nerve tissues and can include heart rate abnormalities, red eye, and weakness and paralysis of the facial muscles (Bell’s palsy). People may develop arthritis months to years after the initial tick bite. And in the late stages of the disease people may have neurological problems such as numbness or tingling in the extremities, memory loss and confusion, Johns Hopkins states.
Lyme disease symptoms appear to be driven mostly by inflammation and immune dysregulation. However, the exact mechanisms behind the condition are not fully understood and remain an active area of research, according to a 2021 review published in the journal Frontiers in Medicine.
If you find a tick on your skin, remove it carefully and fully and clean the affected skin. (Image credit: Getty Images)
How is Lyme disease diagnosed?
Because the symptoms of Lyme disease overlap with those of other conditions, the infection can sometimes be misdiagnosed. For example, some Lyme disease patients are initially misdiagnosed as having shingles, a painful infection caused by the same virus as chickenpox, or with bacterial cellulitis, an infection of the skin caused by bacteria other than Borrelia burgdorferi, Wormser said.
Around 40% of individuals with Lyme disease are diagnosed in the late stages of the infection, according to the Frontiers in Medicine review.
To diagnose Lyme disease, a doctor will take a medical history to see if the person has any known tick bites and whether they were likely exposed to ticks, Wormser said. That’s typically followed with a full body exam, including a thorough examination of the skin. If an erythema migrans rash is found, no Lyme disease testing is needed before beginning treatment, he said.
This is because early in the Lyme infection, when rash symptoms typically appear, the immune system has not yet mounted an antibody response that can be detected with a blood test, so additional diagnostic testing wouldn’t detect any further signs of the infection.
If a rash is absent, doctors perform additional tests to confirm a diagnosis of Lyme disease, according to the review in Frontiers in Medicine.
An enzyme-linked immunosorbent assay (ELISA) test is the standard blood test for Lyme disease and determines whether the immune system has developed antibodies to Borrelia bacteria.
But because Borrelia bacteria are fairly common — they also cause sinus and urinary tract infections — people may carry these antibodies even if they don’t have Lyme disease, Wormser explained. So doctors often do a follow-up blood test called the western blot thattells doctors what antigens, or bacterial proteins, are reacting with Borrelia antibodies. This helps them identify whether a person is infected specifically with B. burgdorferi.
Some people with late-stage symptoms of Lyme disease may also get a polymerase chain reaction, or PCR, test. In this assay, fluid from joints or the spine is analyzed for the presence of genetic material from the bacterium.
(Image credit: Kerrick via Getty Images)
How is Lyme disease treated?
Patients who receive the proper treatment for Lyme disease in the early stages typically recover quickly and completely, the CDC states. Antibiotics like doxycycline and amoxicillin work well against Lyme-causing bacteria and are most effective if promptly administered. Antibiotics are usually given for two to three weeks.
Individuals in later stages of disease may require several courses of oral or intravenous antibiotics, but there is the possibility that symptoms will persist even after treatment. These symptoms are known collectively as post-treatment Lyme disease syndrome (PTLDS), sometimes referred to as chronic Lyme disease.
The frequency of this condition is difficult to estimate, but it appears to be rare. Several research teams had great difficulty recruiting subjects for clinical trials investigating PTLDS, according to a 2015 review published in the journal Infectious Disease Clinics of North America.
Evidence suggests that long-term antibiotic therapy is not helpful for individuals with chronic Lyme disease. Outcomes for patients who receive additional prolonged antibiotic treatment are not better than for those who receive a placebo, and long-term antibiotic treatment for Lyme disease has actually been linked to complications, some that lead to hospitalization or even death, according to the National Institute of Allergy and Infectious Diseases.
Chronic Lyme disease has also been used to describe the illnesses of people who have never been officially diagnosed with Lyme disease.
“The majority of patients that I see who have been treated for chronic Lyme do not show any evidence of ever having had Lyme. They just happen to have the same types of symptoms,” Wormser said. The cause of symptoms in these cases is not well understood and has been the subject of much controversy in recent years, he said.
Lyme disease is most often caused by the bacterial species Borrelia burgdorferi. (Image credit: Callista Images/Getty Images)
How can you prevent Lyme disease?
If you find a tick on your skin, remove it as soon as possible, Wormser said. The CDC recommends grasping the tick’s body as close to the skin’s surface as possible using fine-tipped tweezers; pulling upward with steady pressure and no twisting; and then cleaning the remaining bite wound with rubbing alcohol or soap and water. Do not try to burn the tick off or use chemicals to remove it, Wormser urged.
“If you can get the tick off within 24 hours, you’re not going to get Lyme disease,” Wormser said. You can also bring the tick with you to a doctor’s appointment, he said. A doctor who specializes in Lyme should be able to examine the tick and tell you how long it’s been attached to your skin and whether you’re at risk of Lyme.
Related: Tick-borne illnesses are on the rise. Here’s how to protect yourself.
“You should do a tick check every 24 hours if you’ve been outside,” Wormser said. “To do a good tick check, you really need a second person, because it’s hard for you to see all the areas where the ticks could be biting you.”
Wormser also recommends bathing within two hours of coming inside after being outdoors. Wearing insect repellant on exposed skin and covering up as much as possible when spending time outdoors can also limit exposure to ticks, he said. If you do spend a lot of time outside, try to avoid walking through tall grass, as ticks tend to live in such areas.
Currently, there are no available vaccines for Lyme disease prevention. However, clinical trials are ongoing and several vaccine candidates have shown promising results, according to a 2022 review published in the journal . In addition, researchers have developed a preventative antibody-based treatment for Lyme that is expected to enter trials soon.
This article is for informational purposes only, and is not meant to offer medical advice.