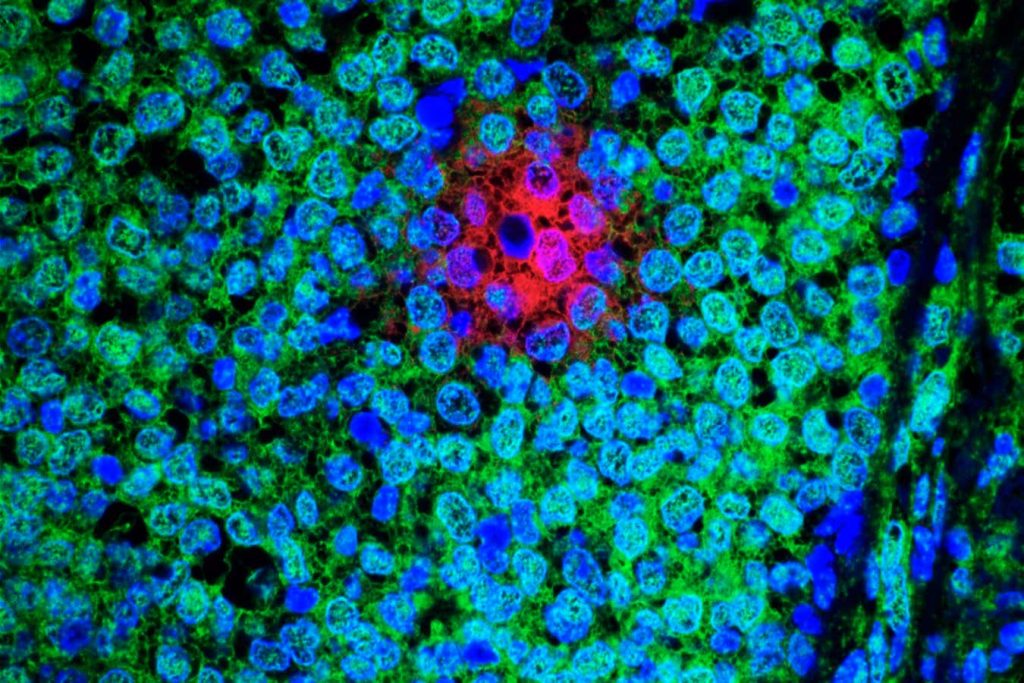
A micrograph of oestrogen-receptor positive breast cancer tissue, showing slowly dividing cancer cells (red) that resist treatment, the cells’ nuclei (blue) and rapidly dividing cancer cells (green)
Dana-Farber Harvard Cancer Center at Massachusetts General Hospital/NATIONAL CANCER INSTITUTE/SCIENCE PHOTO LIBRARY
A repurposed leukaemia drug may be able to stop the most common type of breast cancer from causing tumours elsewhere in the body, according to a study in mice. The drug can cause side effects, however, and there is no way of telling who is most at risk of their breast cancer spreading, which may limit the treatment’s use as a preventative measure for secondary cancer.
Frances Turrell at the Institute of Cancer Research in the UK and her colleagues induced oestrogen-receptor positive (ER+) breast cancer in mice. This is the most common type of breast cancer in humans, accounting for up to 80 per cent of cases, and usually occurs in people over the age of 50.
ER+ breast cancer frequently recurs several years after seemingly successful treatment. This is because the cells can move to other sites in the body prior to treatment and cannot be detected before the therapy is initiated, says Turrell. “These cells essentially stay dormant and then something may trigger them to reawaken them.”
Advertisement
To learn more, the researchers gave young mice – aged 8 to 10 weeks – and older mice – aged 9 to 18 months – ER+ positive breast cancer. The mice, which were all female, weren’t treated for these tumours. Between two and five weeks later, nearly all had cancer cells at secondary sites.
In the young mice, these secondary site cancer cells didn’t divide into tumours, while in the older mice the cells were more likely to develop into tumours, which mainly grew in the animals’ lungs.
The researchers then found that tumour growth in the older mice was linked to an increase in the growth factor PDGF-C in the lungs, which occurred less in the younger mice.
In both people and mice, PDGF-C levels increase in the lungs with age, which may trigger an environment that stimulates secondary cancer cells to divide, says Turrell.
According to Clare Isacke at the Institute of Cancer Research, higher PDGF-C levels may be linked with a weakened immune system.
In another part of the experiment, the researchers partly blocked tumour growth in the older mice after the cancerous cells had spread to the animals’ lungs. This was done by inhibiting PDGF-C using the drug imatinib, which is widely given to people with chronic myeloid leukaemia.
Imatinib inhibited the growth rate of the mice’s secondary tumours, but some lesions did still form, says Turrell.
Although this may have potential for use in people, there is no way to predict whose ER+ breast cancer may later recur elsewhere in their body, she says.
Imatinib has side effects, such as stomach pain and fatigue. “You don’t want to be treating someone who won’t actually experience a relapse,” says Isacke.
The researchers now plan to repeat this experiment in mice using a drug that has a more targeted effect on PDGF-C levels.
Suzanne Wardell at Duke University, North Carolina, says the study highlights the need to better understand the environmental factors in the body that cause a secondary tumour to grow. “Further work is needed to determine the overall general applicability of the findings to human cancer treatment,” she says.
Article amended on 15 March 2023
This article has been changed to correct the sex of the mice in the experiment.
Topics: